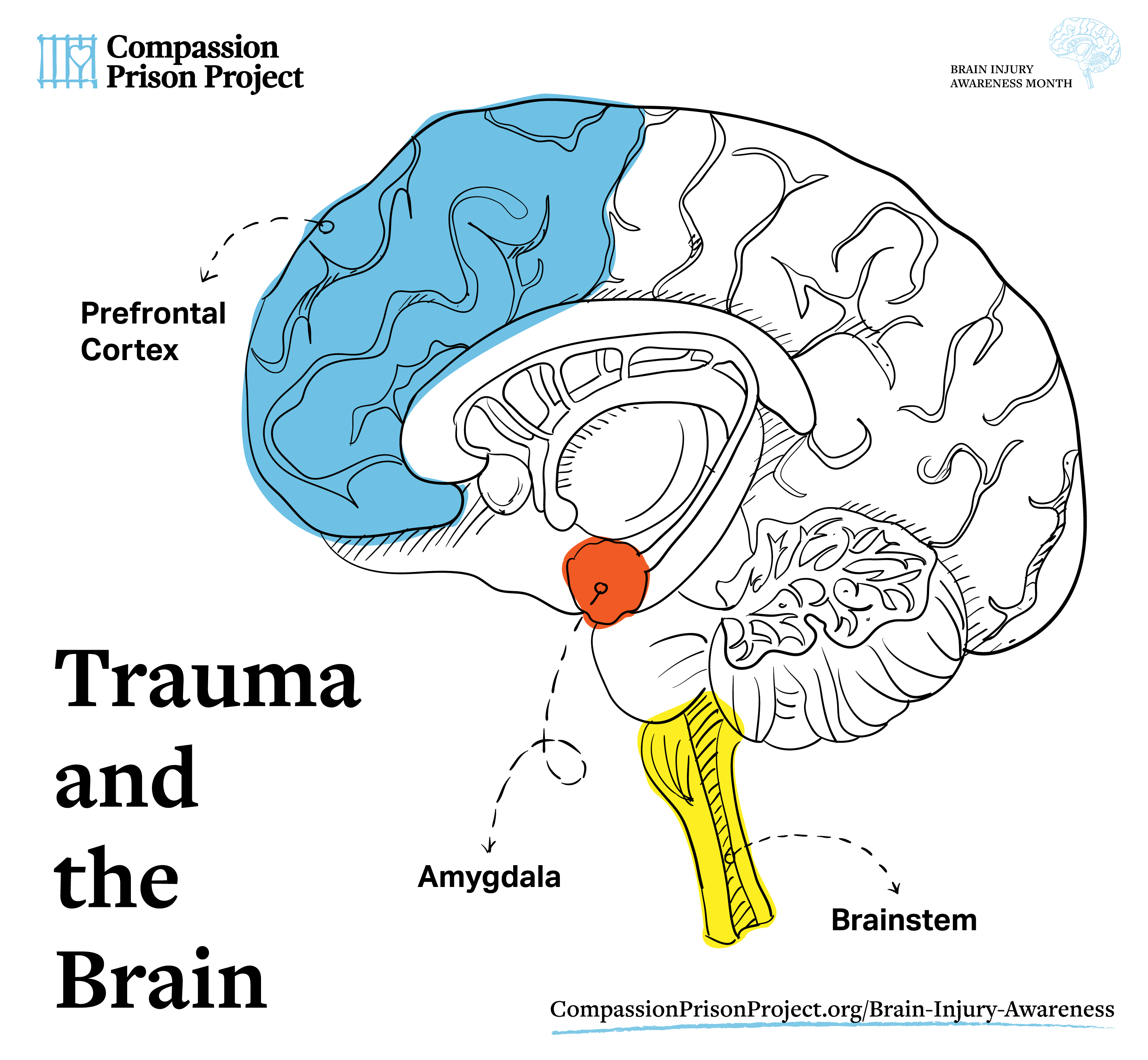
Traumatic Brain Injury (TBI) Affects Everyone. We have created this TBI Awareness Campaign so you can understand the effects of TBI as well as the symptoms and begin to find healing from this injury that may have happened when you were a child or teenager.
Definitions of TBI:
- An insult to the brain caused by an external force that results in an altered state of consciousness and one or more impairments of brain function. The effects may be temporary or permanent.
- Impairments in cognitive abilities such as memory, problem solving and perception.
Leading causes of brain injuries:
- Falls
- Struck by object
- Vehicle Accidents
- Assaults
- Sporting Accidents
The impact of a traumatic brain injury on an individual’s level of functioning afterward depends on the following:
- The severity of the initial injury
- The rate/completeness of physiological recovery
- Which of the brain’s functions are directly affected by the injury
- The meaning of the dysfunction to the individual (in other words, how reliant was the person on those functions before they were lost?)
- Resources available to aid recovery (medical, counseling, etc.)
- What areas of function remain intact and operational after the injury
TBI Symptoms
Brain injuries can range in scope from mild to severe. Traumatic brain injuries (TBI) can result in permanent neuro-biological damage that can, to varying degrees, produce lifelong challenges for the individual.
According to the CDC:
- A brain injury resulting in altered mental status and/or loss of consciousness for up to 30 minutes may be called “mild.”
- Unconsciousness lasting from 30 minutes to 24 hours is associated with brain injuries of moderate severity,
- Unconsciousness lasting longer than 24 hours (coma) are classified as severe.
Dr. Kim Gorgens explains Traumatic Brain Injury (TBI)
Dr. Kim Gorgens is a Professor of Psychophysiology, Clinical Neuropsychology and Psychology of Criminal Behavior at University of Denver. She manages a large portfolio of traumatic brain injury, TBI, related research, and has lectured extensively on those issues, including a 2010 Ted Talk on youth sports concussion, a 2018 Ted talk on brain injuries and criminal justice, several NPR spots, and an interview on CNN with Anderson Cooper. Her work has been featured in US News, Newsweek Salon and more. Her research studies the reported injury history, cognitive function, and brain biomarkers of youth and college athletes, probationers and inmates. Her mission is to better understand the short and long-term impacts of injuring our most vital organ.
Watch: Brain Injuries and Crime – The Startling Connection with Neuropsychologist Dr. Kim Gorgens
Effects of a traumatic brain injury can include:
- ATTENTION – Feeling mentally “foggy”
- CONCENTRATION – Difficulty concentrating
- DISTRACTIBILITY – Inability to focus
- MEMORY – Forgetting recent conversations or information, difficulty remembering
- SPEED OF PROCESSING Feeling slowed down
- CONFUSION – Confused about recent events, difficulty understanding or making sense of the goings-on in the world around you
- FEELING DAZED OR STUNNED
- PERSEVERATION – Continual involuntary repetition of a thought or behavior
- IMPULSIVENESS
- DIFFICULTIES WITH SPEECH AND LANGUAGE:
- Language Processing – Answering questions slowly, repeating questions
- Not understanding the spoken word (called “receptive aphasia”)
- Difficulty speaking and being understood (called “expressive aphasia”)
- Slurred speech
- Speaking very quickly or very slowly
- Problems with reading
- Problems with writing
- HEADACHES
- NAUSEA
- VOMITING
- BALANCE
- PROBLEMS
- FATIGUE
- NUMBNESS/TINGLING IN LIMBS
- MENSTRUAL DIFFICULTIES
- SEIZURES – Involuntary convulsions which can involve disruption in consciousness, sensory perception, or motor movements
- PHYSICAL PARALYSIS/SPASTICITY
- CHRONIC PAIN
- LOSS OF BOWEL AND BLADDER CONTROL
- LOSS OF STAMINA/ENERGY
- APPETITE CHANGES
- POOR REGULATION OF BODY TEMPERATURE
- SLEEP DISORDERS:
- Drowsiness
- Sleeping less than usual
- Sleeping more than usual
- Trouble falling asleep
- DECREASE IN, OR LOSS OF, HEARING ABILITY
- RINGING IN THE EARS (called “Tinnitus”)
- INCREASED SENSITIVITY TO SOUND OR LIGHT
- PARTIAL OR TOTAL LOSS OF VISION
- WEAKNESS OF EYE MUSCLES AND DOUBLE VISION (Diplopia)
- BLURRED VISION
- PROBLEMS JUDGING DISTANCES VISUALLY
- INVOLUNTARY EYE MOVEMENTS
(called “Nystagmus”) - INTOLERANCE OF LIGHT (called “Photophobia”)
- LOST OR DIMINISHED SENSE OF SMELL (called “Anosmia”)
- LOST OR DIMINISHED SENSE OF TASTE
- INABILITY TO FILTER SENSES,
- EASILY OVERLOADED
- DIFFICULTY WITH THE INTERPRETATIONOF TOUCH, TEMPERATURE, MOVEMENT, LIMB POSITION
- DEPENDENT BEHAVIORS (needing to rely on help from others to accomplish tasks)
- EMOTIONAL LABILITY (mood swings, unpredictable emotional displays, intense moods)
- LACK OF MOTIVATION
- IRRITABILITY
- SADNESS
- NERVOUSNESS
- AGGRESSION
- DEPRESSION
- DISINHIBITION/IMPULSIVITY
- DENIAL/LACK OF AWARENESS
TBI is associated with an increased risk for irritability, temper outbursts and decreased self control in addition to cognitive problems such as attention and memory. Five years after a severe brain injury, 64% were described as having a bad temper and 54% threatened violence.
While a person may have been calm and controlled before their injury, afterwards they may become quick-tempered and lack inhibition. TBI also increases the risk for psychiatric disorders and substance abuse. Studies indicate that abusive experiences in a person’s life tend to increase the inclination toward violence after brain impairment.
Supporting incarcerated individuals with TBI
50% – 80% of people in prison have experienced some form of TBI. When we look at the female population that number jumps to as high as 97%. This is mainly due to the act of strangulation. A lot of domestic violence results in strangulation which can injure the brain.
Challenges which are unique to the prison setting arise for incarcerated individuals with a TBI. These challenges may include:
- Having difficulty understanding directions
- Appearing to be slow or unresponsive to staff requests
- Having trouble remembering instructions from staff
- Acting impulsively with staff or other incarcerated individuals
- Having difficulty organizing one’s cell and keeping it tidy
- Having rapid mood swings with no apparent reason, making a person more volatile in public spaces
- Responding too aggressively to other incarcerated individuals or staff
- Having anxiety or depression and withdrawing from social interaction
- Being more sensitive to lights and sounds, especially in crowded common areas
Brain-Derived Neurotrophic Factor (BDNF)
The best thing you can do to help heal your brain, is get out and exercise! Exercise helps heal the brain. Running, jogging, sprinting, weight-lifting, burpees and any other cardiovascular exercise helps promote the production of Brain-Derived Neurotrophic Factor (BDNF) in the brain.
“BDNF is like Miracle Gro for the brain.”
— Dr. Kim Gorgens, Neuropsychologist
Researchers have found that a single session of exercise can increase the BDNF protein in the brain. It is about creating cardiovascular demand—getting your heart rate up for even a short time—in animals, that is 60 seconds which is an attainable goal for most of us!
Make cardiovascular exercise part of your every day routine.
Summary
Traumatic Brain Injury in prison is common. Up to 80% of prison residents have TBI. (In some prisons that number is as high as 87% and in women’s prisons, it can go as high as 97%.)
Having a TBI can make it difficult to think clearly and communicate to people what’s going on. Awareness that you have suffered a TBI and that it has affected you, is key to maneuvering through prison. Letting people you are living and working with know that you have trouble perhaps with understanding things or hearing things or remembering things can change (among other issues) the outcome of your time in prison — lowering the stress and frustration that can happen when someone is misunderstood.
Being aware of the issues surrounding Traumatic Brain Injury helps you and your environment become “trauma-informed” and can help your community become more understanding and compassionate towards our own limitations. Healing is possible, we just need to know that we’re injured in the first place.